These metabolism test results represent years 15-18 of drinking 40g of traditionally prepared kava per day.
You can see my first test was crazy as I had just gotten out of the hospital w/ covid. Wasn’t fun, and those tests reflect it.
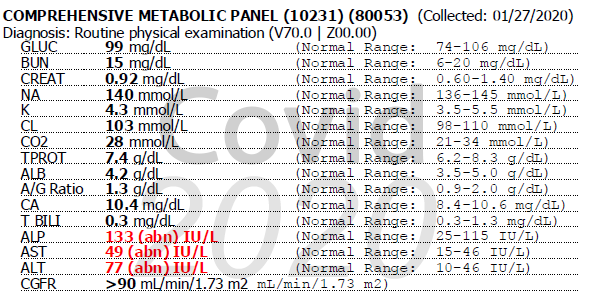
My ALT/AST values were not good. Consequently I actually started BACK drinking kava during the time of that test after my release from the hospital, and you can track the changes to my subsequent test that year (90 days later) with normal ALT/AST values for liver histology.
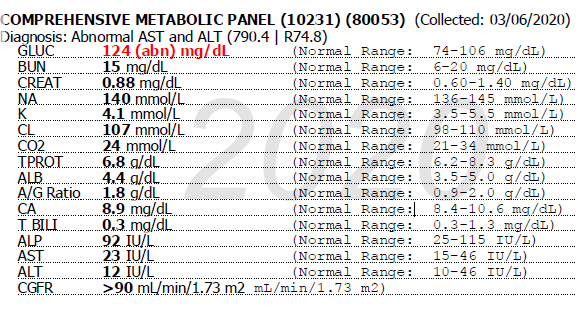
Essentially I drank kava even when my liver was in peril and nothing came of it. Remember I am a study of ONE, so this in no way writes the book, but it’s some rather strong evidence that kava in fact did not cause any type of liver stress even on top of a stressed liver.
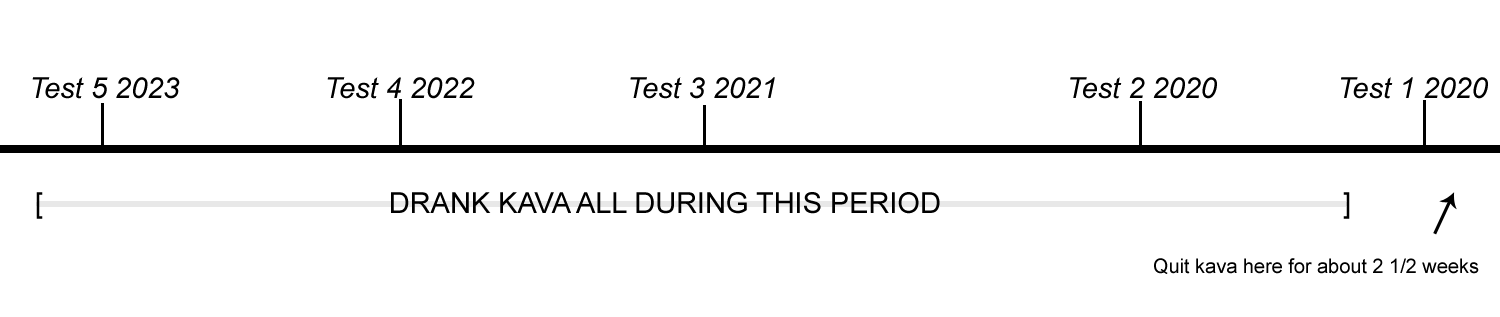
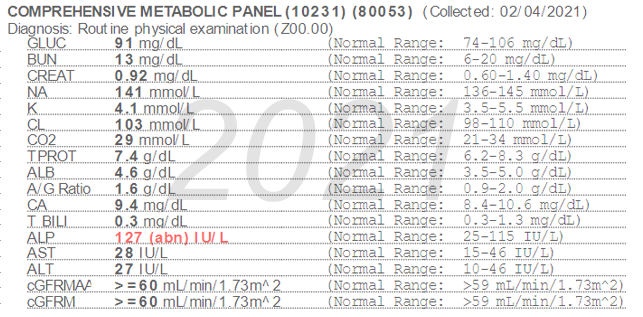
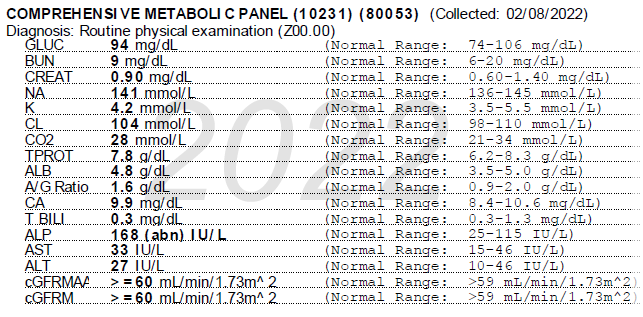
As you can see I’ve only had one test where ALP levels were within normal range indicated on the 2nd test from 2020, 3 months after the first. Rises in ALP without corresponding GGT increases (GGT was normal) indicate non-hepatic causes (Limdi et al 2003). Not only this, but the level of increase is/was less than 2 times the upper normal limit, indicating a non-damage condition. Considering there are no rises in GGT, ALT, AST, or Bilirubin we can conclude this has nothing to do with the liver itself, and also is not an indicator of any liver damage (Francher et al 2017). We first thought this was due to my vitamin D levels, which were abysmal. After supplementation for a year my vitamin D levels are now over the upper limit, and my ALP, while lower than last year, is still slightly in the high range. Now, with all of this information in hand, I’m a bit more comfortable saying that this ALP rise is likely an artifact of my kava consumption…possibly. Not a medical doctor, so of course I can’t say for absolute sure. I do take a couple of other prescription drugs, however I was definitely not taking those at the first test. None of the drugs I take regularly have any history of causing this pattern of ALP elevation.
The evidence is tenuous, but Clough et al in 2003 found GGT and/or ALP rises without corresponding AST/ALT, bilirubin, or any other liver damage markers in daily kava drinkers. This was seen in kava consumption at levels of over 118g per week. I fall into this category squarely at 280g per week consumption. Are they connected? Hey, maybe they are. My doctor says it’s nothing to be concerned about and we’ll just watch it.
Clough, Alan R., Ross S. Bailie, and Bart Currie. 2003. “Liver Function Test Abnormalities in Users of Aqueous Kava Extracts.” Journal of Toxicology. Clinical Toxicology 41 (6): 821–29. https://doi.org/10.1081/clt-120025347.
Fancher, Tonya, Amit Kamboj, and John Onate. 2017. “Interpreting Liver Function Tests.” Current Psychiatry 6 (5): 61–68. https://paperpile.com/app/p/94c842a5-c415-049f-9f18-7102b77b940b
Limdi, J. K., and G. M. Hyde. 2003. “Evaluation of Abnormal Liver Function Tests.” Postgraduate Medical Journal 79 (932): 307–12. https://doi.org/10.1136/pmj.79.932.307.
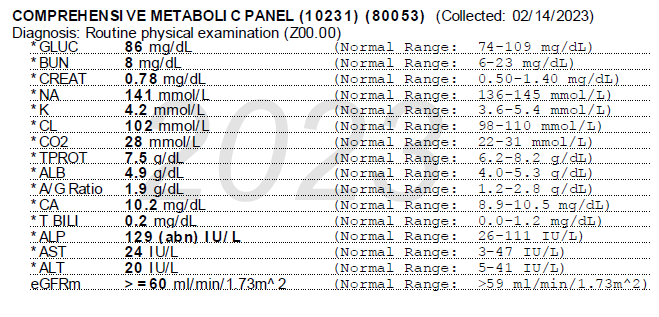
You can see my first test was crazy as I had just gotten out of the hospital w/ covid. Wasn’t fun, and those tests reflect it.
My ALT/AST values were not good. Consequently I actually started BACK drinking kava during the time of that test after my release from the hospital, and you can track the changes to my subsequent test that year (90 days later) with normal ALT/AST values for liver histology.
Essentially I drank kava even when my liver was in peril and nothing came of it. Remember I am a study of ONE, so this in no way writes the book, but it’s some rather strong evidence that kava in fact did not cause any type of liver stress even on top of a stressed liver.
As you can see I’ve only had one test where ALP levels were within normal range indicated on the 2nd test from 2020, 3 months after the first. Rises in ALP without corresponding GGT increases (GGT was normal) indicate non-hepatic causes (Limdi et al 2003). Not only this, but the level of increase is/was less than 2 times the upper normal limit, indicating a non-damage condition. Considering there are no rises in GGT, ALT, AST, or Bilirubin we can conclude this has nothing to do with the liver itself, and also is not an indicator of any liver damage (Francher et al 2017). We first thought this was due to my vitamin D levels, which were abysmal. After supplementation for a year my vitamin D levels are now over the upper limit, and my ALP, while lower than last year, is still slightly in the high range. Now, with all of this information in hand, I’m a bit more comfortable saying that this ALP rise is likely an artifact of my kava consumption…possibly. Not a medical doctor, so of course I can’t say for absolute sure. I do take a couple of other prescription drugs, however I was definitely not taking those at the first test. None of the drugs I take regularly have any history of causing this pattern of ALP elevation.
The evidence is tenuous, but Clough et al in 2003 found GGT and/or ALP rises without corresponding AST/ALT, bilirubin, or any other liver damage markers in daily kava drinkers. This was seen in kava consumption at levels of over 118g per week. I fall into this category squarely at 280g per week consumption. Are they connected? Hey, maybe they are. My doctor says it’s nothing to be concerned about and we’ll just watch it.
Clough, Alan R., Ross S. Bailie, and Bart Currie. 2003. “Liver Function Test Abnormalities in Users of Aqueous Kava Extracts.” Journal of Toxicology. Clinical Toxicology 41 (6): 821–29. https://doi.org/10.1081/clt-120025347.
Fancher, Tonya, Amit Kamboj, and John Onate. 2017. “Interpreting Liver Function Tests.” Current Psychiatry 6 (5): 61–68. https://paperpile.com/app/p/94c842a5-c415-049f-9f18-7102b77b940b
Limdi, J. K., and G. M. Hyde. 2003. “Evaluation of Abnormal Liver Function Tests.” Postgraduate Medical Journal 79 (932): 307–12. https://doi.org/10.1136/pmj.79.932.307.
